※This is Puchiko’s experience and isn’t a substitute for diagnosis or treatment.
I think I’ll take the liberty of explaining the kidney biopsy that Puchiko underwent, based on what I witnessed. What images come to your mind when you hear the term Kidney Biopsy? I made sure to observe Puchiko’s procedure closely. I know that those who actually have to undergo a kidney biopsy must feel anxious. I’d like to share Puchiko’s firsthand experience with the procedure.
Table of Contents
1. Who Needs a Kidney Biopsy?
What is a kidney biopsy? If I just told you to refer to the many chronic kidney disease survivors who write about this elsewhere, you’d think I was lazy. So, let’s be thorough.
First, let’s talk about the select few who undergo a kidney biopsy. Since Puchiko lives in Japan, I will share the Japanese criteria here.
1) When there is 0.3–0.5g or more of proteinuria per day.
Puchiko had urine soaked in protein more than any other renal disease (same as her) patient, excreting about 40 times more urine protein than normal.
2) When a massive amount of proteinuria is observed (e.g., Nephrotic Syndrome).
3) When there is acute kidney failure (a state where the kidney’s filtration function worsens over a week).
The condition where acute renal failure is accompanied by blood in the urine is called “Rapidly Progressive Glomerulonephritis (RPGN).” This often occurs due to systemic diseases and requires prompt diagnosis and treatment.
4) When diagnosing the cause of unexplained renal failure without hematuria or proteinuria.
5) For diagnosing the cause in a transplanted kidney.
Of course, even if you meet the above criteria, you may not be able to undergo a kidney biopsy. For instance, if:
• The kidneys are atrophied or there is a size difference between the left and right kidney according to an ultrasound.
• A bleeding tendency cannot be controlled.
• There is an infection in the kidney itself or the surrounding area.
• There are morphological abnormalities in the kidney, such as Polycystic Kidney Disease (PKD).
• The patient cannot comply with instructions during the examination or maintain post-examination bed rest.
• The patient does not wish to or cannot give consent.
Also, the doctor told Puchiko that patients with only one kidney cannot have the biopsy.
2. Why Do They Do a Kidney Biopsy for Renal Disease?
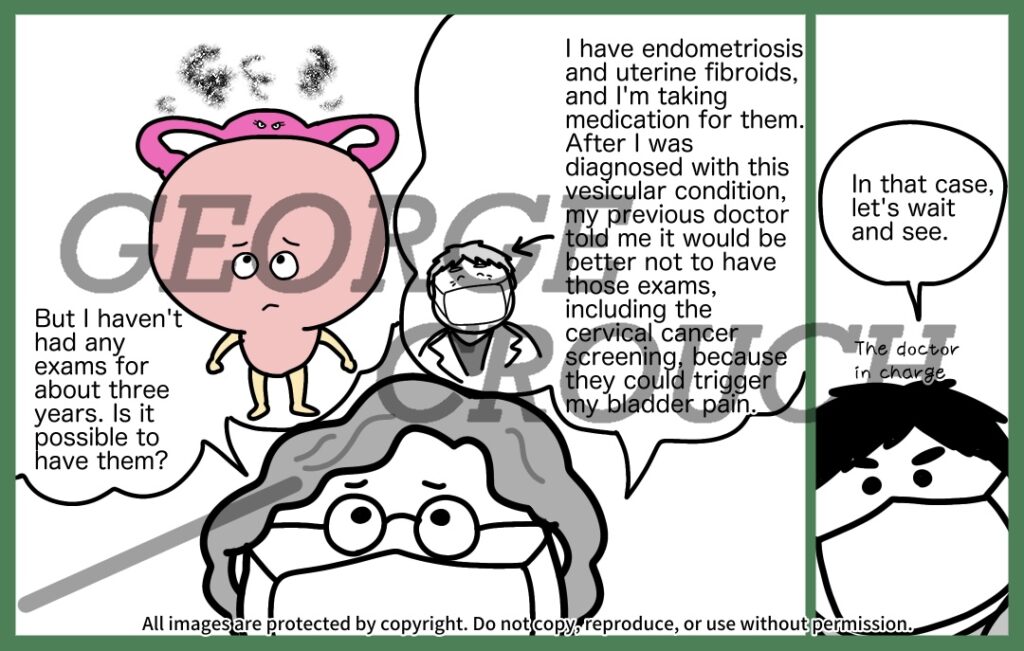
Puchiko’s failure to undergo the biopsy initially, only to later receive unsuccessful treatment, is a perfect example of its necessity. Most her renal disease patients likely follow the sequence: Kidney Biopsy → Tonsillectomy → Steroid Pulse Therapy.
However, Puchiko’s former doctor said, “In my gut feeling, after 40 years at [a famous university hospital], you have renal disease. Your hematuria won’t disappear.” Based solely on that gut feeling, Puchiko underwent a tonsillectomy but was only treated with medication for blood clots, hyperlipidemia, and high uric acid.
Two years passed without any drugs effective against renal disease. And what happens to people in such a state? “You’re just losing time and money without knowing the correct status! Achieving remission after the disease has progressed takes more time and money! Is that okay? Do you want to end up like Puchiko? The reason you need the biopsy is precisely so you don’t end up like her. Decide on treatment based on data, not a gut feeling!” I want to scream this to my readers. Don’t you feel the necessity? Don’t the words of someone who failed penetrate to your very core?
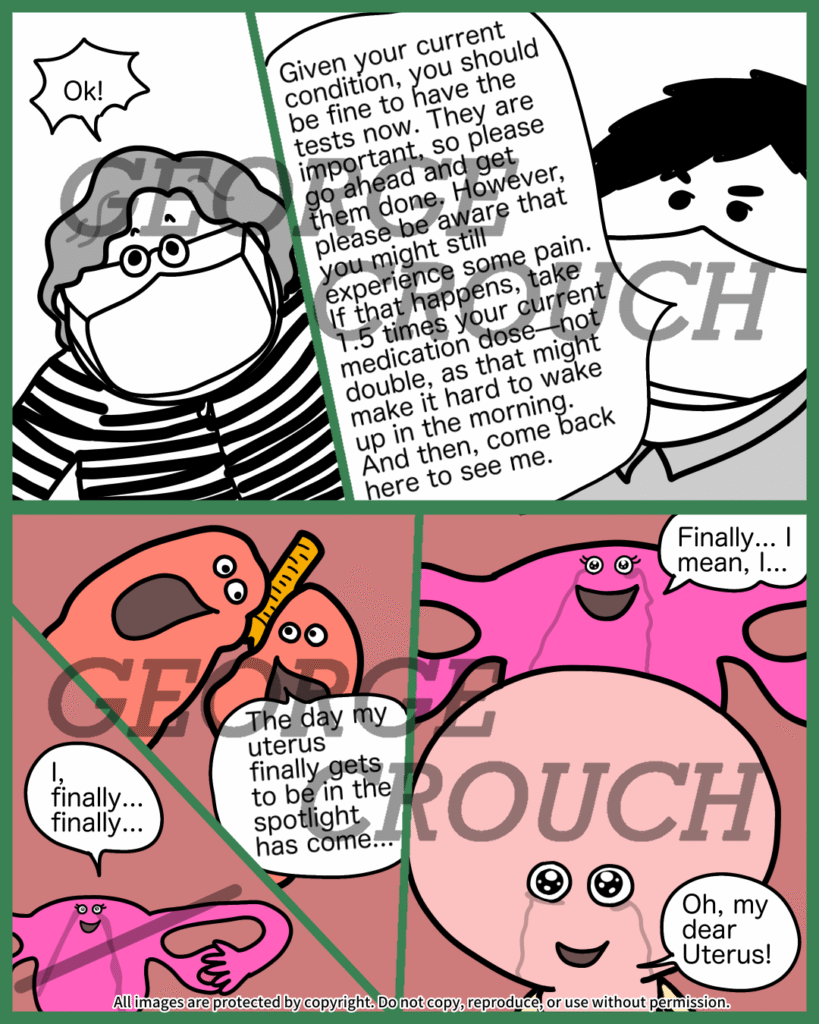
To reiterate the necessity of the kidney biopsy: it reveals the current status of your kidneys. If normal is Grade 0 and mild renal dysfunction is Grade 1, then renal failure is Grade 4. When Puchiko finally had her kidney biopsy, she was at Grade 2. The biopsy shows how much the kidney tissue has been threatened by I g A. This detailed status allows doctors to tailor the treatment accordingly. There is so much information you can’t get from just urine and blood tests alone.
Did I manage to convey the need for the biopsy? From here, I’ll share Puchiko’s experience of the procedure.
3. The Procedure
As a prologue, before the kidney biopsy (which was before her hospitalization in Puchiko’s case), an ultrasound is performed to check for kidney atrophy, left-right size differences, or morphological abnormalities. To prepare for bleeding, anticoagulant drugs (so-called “blood thinners”) are stopped. Since she was taking them for clot prevention, Puchiko had to go without them during the biopsy hospitalization.
There are two methods: local anesthesia in the patient room/ward (which Puchiko had) or general anesthesia in the operating room.
For the procedure: Since movement is strictly prohibited for 24 hours after the biopsy—even for going to the bathroom—a urinary catheter is placed. Puchiko said this was the most painful part of the entire kidney biopsy. She was furious at me afterward. I apologize. I don’t want to shock you with the word “painful,” but it is painful. Why? Because in her case, the attempt failed four times, and the catheter was removed and reinserted once. It was a tragedy.
Now, for the main event. She was moved to the specialized room on her bed. Lying face down, her back was heavily slathered with Iodine (like applying a massive amount of toner). Three doctors, three nurses, and one person who looked like a technician—many eyes were fixed on Puchiko’s iodine-coated back and waist area. They use an ultrasound to observe the kidney’s shape, and multiple doctors determine the needle insertion point. After injecting local anesthetic into the skin, a thin needle (about the size of a ballpoint pen tip) is inserted through the back, and anesthetic is injected onto the surface of the kidney once the needle reaches it.
The doctor says, “Now, I will insert the needle… Take a breath in—Now! Hold your breath completely.” A loud thwack sound is heard. The needle enters the kidney, and a small piece of the kidney is collected. The tissue is about the thickness of a pencil lead and 1 to 2 cm long. I was watching the whole thing from behind and got goosebumps.
Only one kidney is tested; in Puchiko’s case, it was only the left one. The technician checks the collected tissue under a microscope to ensure the desired sample is included. If it’s insufficient, the collection is restarted. (Puchiko’s collection was restarted.) After the biopsy ends, the area is compressed for about 10 minutes while lying face down to stop the bleeding. The doctor’s pressure was so strong I worried Puchiko’s body might literally crack.
After hemostasis, she had to lie on her back for 24 hours of strict bed rest, without moving at all. She survived by using a straw attachment for her water bottle. Since Puchiko couldn’t eat by herself, a nurse assisted her with her meals. She had the biopsy in the early afternoon, and by 6 PM, she was allowed to raise the head of the bed slightly to a seated position.
4. About the Pain
The kidney biopsy itself involved only a slight prick from the anesthetic injection, and apparently, there was no pain from the needle stabbing the kidney. She had been told, “It’s going to hurt,” so Puchiko expected pain after the anesthetic wore off, but she described the pain level as a “refreshing, wasabi-like sting.” Many survivors say that the absolute bed rest is the hardest part, and nurses warned her about the difficulty, but Puchiko didn’t find it hard at all. People with chronic lower back pain might find it tough, though, as lying on your back puts a strain on the lower back.
5. Coping During Absolute Bed Rest and Things to Note
What did Puchiko do during her absolute bed rest? She listened to podcasts on Spotify: Kemio’s Ear Cleaning Club and The Fabulous World of the Kano Sisters (which were airing then). Lying in her large shared room bed, she was laughing so hard she was silently rolling around—well, she couldn’t actually roll around because of the bed rest, but she looked like she was having fun.
I know some of you reading this are worried: “What if it hurts?” “What if the results are bad?” The kidney biopsy hospitalization is just one or two days of enduring the procedure plus the stress of being hospitalized. But it reveals the path you must take next. Instead of being consumed by worry, you understand what needs to be done. Even if the results are bad, you now have a treatment plan to assemble. Knowing this brings true peace of mind. To be freed from vague, frustrating anxiety, this is a time you absolutely must overcome. We, too, are on the other side of this challenge. We wholeheartedly support you.
You Might Also Like