About a year ago, Puchiko traveled to Australia. I observed closely that even with dietary restrictions and health management challenges due to renal disease and vesical condition, as well as aerophagia (air swallowing), Puchiko—who lives with these limitations—could successfully manage an overseas trip without drastically changing her usual lifestyle, provided she planned carefully. I’ve written down her experience here.This is Tips about Overseas Trip with Restrictions. This is the continuation of the previous Part 1
Table of Contents
1. Day 2 with Overseas Trip with Restrictions
Puchiko decided to take the scenic railway to Kuranda, a famous tourist spot she had also visited during her working holiday. She pre-booked the train, which made it slightly cheaper.

The blue train connecting Cairns and Kuranda.

The scenery visible from the window on the way to Kuranda.

The koalas in Kuranda.
When she arrived in Kuranda, Puchiko took a commemorative photo with a koala for the third time in her life. This time, she also took a picture with a python. A large number of Japanese tourists were there, but while everyone took photos with the koalas, she was the only one posing with the python. When I asked her what she thought, she said the python was cool, soft, and surprisingly pleasant to the touch. The python in the picture with her was a white and orange female. She was very cute and had a service-minded nature, giving a direct camera look.

The stylish white and orange python that posed for a photo with Puchiko.
After touring Kuranda, Puchiko was about to have lunch, but she felt something was off. She had started feeling unwell around the time she boarded the train at Cairns Central Station. She ordered dal curry but after three bites, she suddenly felt nauseous and rushed to the restroom. Since I couldn’t follow her inside the restroom, I waited outside, but she told me later that she had vomited.

The gate of the Kuranda Rail Station.
By the time she boarded the return train, Puchiko was completely worn out. In fact, she had lost about 3 kg (6.6 lbs) of weight just before the trip. The malaise had already surfaced when she ate chanpon at Narita Airport. Although she was wearing a mask, she unfortunately slept with her mouth open on the train and ended up with a sore throat. It was regrettable, considering how carefully she managed her health on the plane. This incident made her decide that she must also carry nasal breathing strips for times when she might accidentally fall asleep while outside. When she returned home, completely exhausted, a cute visitor had arrived.

The light-colored calico cat that visited Puchiko’s doorstep.
2. Day 3 with Overseas Trip with Restrictions
Despite being worn out, Puchiko had to wake up at 1:00 AM. She got ready and walked through the dark to the bus stop near the Botanical Garden to wait for her bus. This was because Puchiko had booked a hot air balloon ride early in the morning. Puchiko was the first passenger on the bus; all the subsequent passengers were Japanese tourists staying at hotels. She thought, “They must be rich.”
Just when she was feeling unwell, she got motion sickness, and Puchiko vomited as soon as she arrived at the site. The plastic bag she had brought came in very handy that day.
Once in the hot air balloon, she certainly enjoyed the view, but being quite petite (as her nickname ‘Puchiko’ implies), a couple that was quite large for Japanese people stood in front of her. When they took commemorative photos, she didn’t show up in the pictures. Naturally, I, Puchiko’s imaginary friend, didn’t appear either.

The early morning sky photographed from a hot air balloon.
After landing, there was time for a light meal, and though Puchiko didn’t eat, she was thirsty and accepted a drink. The only non-alcoholic option was orange juice, but what she was handed was actually champagne mixed with orange juice by mistake. The moment she drank it, she immediately felt sick and struggled repeatedly to hold back the vomit. On the bus ride back, she vomited quite a bit. However, learning from the previous day’s mistake, she kept her nasal breathing strip on and wore a mask during the hot air balloon ride and the bus ride, only removing them to vomit or drink water.
When she got home, all Puchiko ate was one pack of strawberries. This could hardly be called self-catering. Her throat hurt even more from the vomiting, so she sucked on a medicinal candy-like lozenge she bought at COLES (supermarket) and spent 12 hours sleeping and resting.

The half-eaten strawberry that was the only food Puchiko could manage to eat.

The lozenge that caused a numbing sensation and suppressed inflammation when licked.
3. Day 4 with Overseas Trip with Restrictions
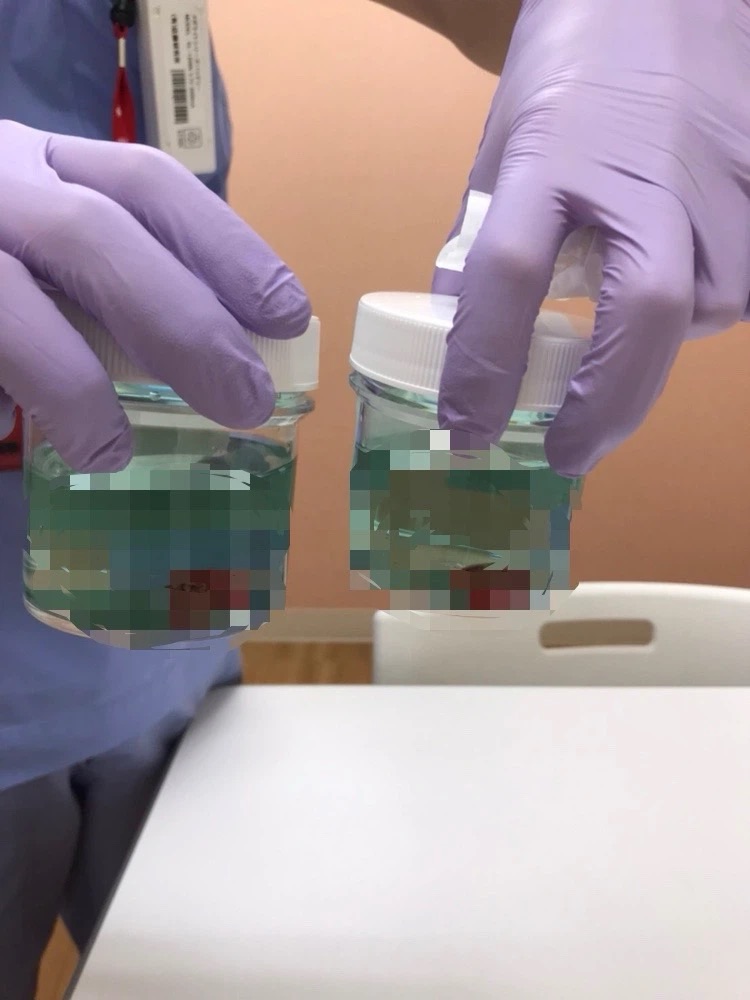
After a good night’s sleep, Puchiko’s sore throat had disappeared. If she hadn’t had her tonsils removed, she might have had a high fever and blood in her urine right now.
For breakfast, Puchiko ate homemade asazuke (lightly pickled veggies), white rice, and homemade miso soup. She decided to go sightseeing in the city that day. She walked past a nightclub she used to frequent on Friday nights during her working holiday days. It felt like a world completely separate from her current life, where she goes to sleep at 8 PM. She continued walking and looked out at the Esplanade.

The kangaroo road sign near the Airbnb.

The Esplanad.

The weekend market

The half melon bought at that market.
She went to a market that only opens on weekends and bought a melon. A half-cut melon was A$2 (¥200). In Japanese supermarkets, they usually cost ¥1,000 (A$10) to ¥2,000 (A$20).
Next, Puchiko went to the casino. You can enter by showing your ID to the guard. Slots seem to be available during the day, but table games only start in the evening. During her working holiday, someone from her language school was strapped for cash and earned A$100 gambling at this casino.

The dazzling casino
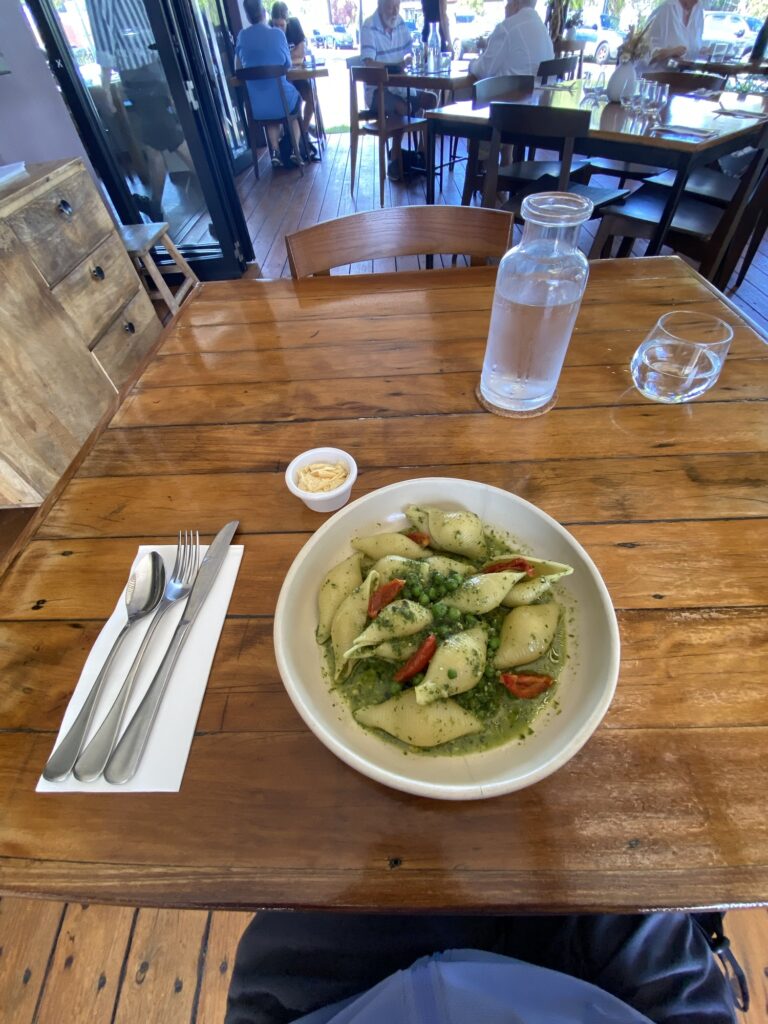
Puchiko returned home and cooked Dandan Noodles for lunch using brown rice noodles and oat milk. Rice flour allows for lower protein intake than wheat flour, and oat milk allows for lower protein intake than soy milk. Since some vesical condition patients seem to experience inflammation from soy products, this substitution is recommended for them. However, it’s hard to find additive-free oat milk in Japan. Irritants are also bad for vesical condition, so she added a small amount of shichimi chili pepper to make it only mildly spicy. She then indulged in the half-cut melon she had just bought at the market. Melons are high in potassium, so those with kidney disease requiring potassium restriction should refrain from such recklessness.
Afterward, Puchiko strolled through the Botanical Garden near her Airbnb. However, as the clouds show, it became a squall, so she rushed back home. As I wrote in a previous article (【Mental Health】Ultimate Guide to Clinic Stress Relief and Finding Peace in Nature), she enjoys strolling through nature in various places because the plants and animals that inhabit them are different. After returning home, she made and ate Tomato Pasta using brown rice noodles, and then went to sleep.

The Botanic Gardens

The road near the Airbnb, which Puchiko used to walk often when she lived in this neighborhood for her homestay.

The lake in the Botanic Gardens.
4. Day 5 with Overseas Trip with Restrictions
Since she was returning home the next day, she needed to use up her ingredients. For breakfast, she cooked and ate zousui (rice porridge). She decided that this day would be for souvenir shopping. She would have preferred the Night Market, but as the name suggests, it only opens after 4 PM. Being located outside the city center, she felt it was too much hassle… plus, she gets sleepy in the evening. She decided to buy souvenirs at a souvenir shop in the city center starting in the morning.
The benches in the city center are decorated with Aboriginal art. The trees in the city are full of bats! Tourists try to take photos, but beware of droppings, which are full of germs!
Puchiko returned home and cooked and ate Tanmen (salt-based ramen with veg) using brown rice noodles. Afterward, she took a walk near the Airbnb to the area where her former homestay was located.
Back then, Puchiko shortened her homestay period compared to what was planned. She grew disgusted because the host father would touch her feet with his bare feet during meals, told her a rotten tangerine was “just for her,” called her with a whistle like calling a dog, and the separated son (who was her age) brought his girlfriend over every night and made noise, plus the host mother was hysterical. She quickly moved to a share house.
For dinner, Puchiko cooked a bean soup and ate it with white rice.
6. Return Home
Breakfast on the day of her return was the leftover bean soup from the previous night and white rice. After eating and getting ready, Puchiko checked out. She called an Uber and headed to the airport.

The view from the Airbnb window.

Before boarding
The lasagna served as the in-flight meal… the salt content was outrageous. Puchiko had to wash it down with a massive amount of water. I wouldn’t recommend it to anyone with kidney disease! Since she skipped dinner, she probably managed to keep her daily salt intake within the limit.
7. Message
Overall, unexpected things happened in the first half of the trip, and it seems the flow was different from what Puchiko had anticipated. However, I observed that she was able to enjoy her overseas trip while skillfully controlling her dietary restrictions due to renal disease and vesical condition. When you are in the middle of treatment, it’s easy to think negatively; she was no exception. But I believe that by finding ways to enjoy life through careful planning, a brighter path can open up. While there is no need to force yourself to be positive, I learned from her that deciding on something you want to do and preparing for it and experiencing it can become energy for the soul.
Though it’s still a ways off, Puchiko is planning a trip to Belgium in 4 months, and I intend to write about that next Overseas Trip with Restrictions.