※This is Puchiko’s experience and isn’t a substitute for diagnosis or treatment.
When I thought of a tonsillectomy, my image of it was immediately associated with pain. Of course, I haven’t personally experienced a tonsillectomy or the pain that comes with it. However, I was there to witness Puchiko undergoing the procedure and experiencing the recovery pain, and I would like to share my perspective on that time with you all.
1. Why Do They Do Tonsillectomy?
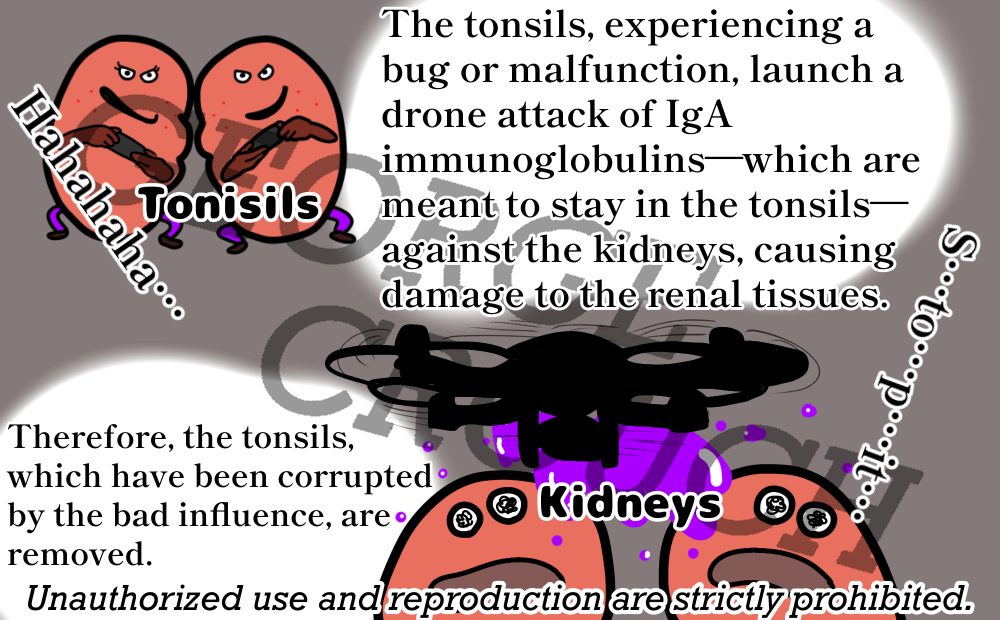
It’s a mystery: the protagonist is the kidney, yet they take out the tonsils… For those of us living with the disease, we understand it. But when you tell a colleague or acquaintance, “I’m having my tonsils out because of a kidney disease,” I’m sure Puchiko and I aren’t the only ones who get a puzzled look and feel too lazy to explain it. Even if I carefully explained, “The cause of renal disease is often a focal infection far from the kidneys, such as tonsillitis, chronic nasopharyngitis, or periapical periodontitis, so we remove the tonsils,” they’d likely just say, “Huh? Doesn’t make sense.” That’s too much hassle.
2. Pre-Surgery Preparation, Flow, and General Details
For the hospital stay, unlike the kidney biopsy, there’s no strict bed rest or no-shower rule, so you don’t need dry shampoo. The most essential item you do need? Tissues, towels, and anything you can spit saliva into! One box of tissues is a ridiculously inadequate amount. Saliva continuously overflows, so much so that I wondered if Puchiko had dehydrated herself by constantly spitting.
3. About the Surgery
Now, about the tonsillectomy itself: on the day of the surgery, Puchiko fasted and was given oral rehydration solution. In her case, she didn’t have a urinary catheter, but some people do, so individual differences exist.
Puchiko walked to the operating room herself. She sat on the operating table and held out her arm to have a needle inserted—but they tried to insert it into the back of her hand instead. The needle failed to go in the first time, and after being poked repeatedly, she took off the oxygen mask she was wearing and angrily said, “That hurts!” I told her, “Puchiko! Endure it!”
Once under general anesthesia, Puchiko dreamed. As her imaginary friend, I was able to experience the dream too, so I stayed in her dream while waiting for her surgery to end. It was a dream about a Pokémon, Gyarados. Since the surgery lasted about two hours, she was woken up mid-dream with, “It’s over now,” and experienced a moment of weightlessness while being transferred to her bed. At that point, she was still groggy and not in pain.
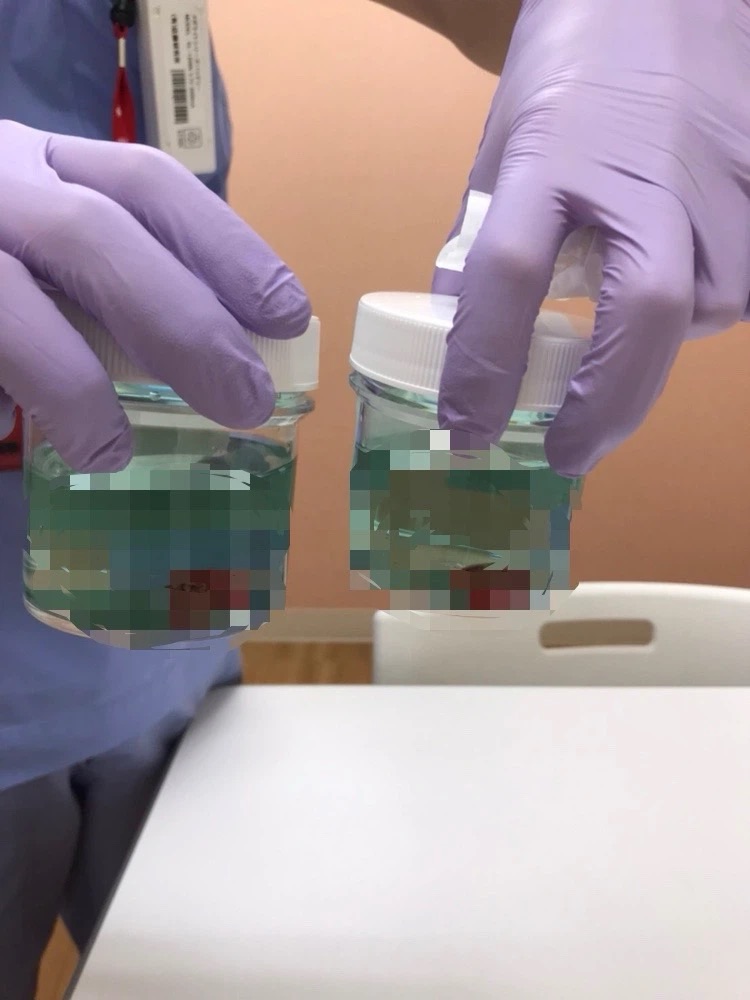
As for Puchiko’s tonsils: before the surgery, we asked the surgeon if her family could take pictures, and her mother did. Looking at the post-op tonsil area, it was whitish. Puchiko was told her tonsils were in the second state out of three stages. The second stage meant they were quite enlarged, and the holes were rather uneven and bumpy. That makes sense, as she used to be able to clear tonsil stones herself, although that’s something you definitely shouldn’t do.
4. Post-Operative Course
She looked comfortable while wearing the oxygen mask after being transferred back to the bed. I assume this was because the anesthesia was still working. After the anesthesia wore off and the oxygen mask came off, Puchiko realized the pain, and that’s where the “hell” began. Ah, maybe I shouldn’t use the word ‘hell,’ but that’s how Puchiko described it at the time. I’ll cover the pain in detail later; here, let’s focus on the recovery process.
She had a low-grade fever post-op. On the second day, her uvula was swollen. She wanted to be discharged quickly, so she asked the doctor what determined the discharge timing. He told her it was when the scabs were firmly in place, the wound was closed, and there was no bleeding.
However, for some reason, they served her crackers (senbei) with her meal. She ate it because it was served, which caused a tear and bleeding, and the doctor got angry at her. When she complained to a more senior visiting doctor, saying, “I ate it because it was served… please don’t serve food we can’t eat,” I remember the doctor saying, “That’s a valid point.” I agreed.
In any case, Puchiko was desperate to be discharged quickly. That’s because the hospital she stayed at for the tonsillectomy served food that was so unappetizing that when she went on a hunger strike, she was scolded. Incidentally, they gave her kiwi fruit, and when she ate it, she felt a pain so intense it hurt the back of her ears and her head. That might have been the most painful moment.
If you want to be discharged quickly, be sure not to injure the surgical site like Puchiko did! Keeping the area from drying out is also important.
5. About the Pain
I used the threatening phrase “where the hell began” earlier, and here, “pain” accounts for most of that hell. However, when I asked Puchiko, she rated the pain level as 2.5 out of 5. …But the constant overflowing saliva was also quite tough. It hurts too much to swallow the saliva, which is why you end up having to spit it out like a spitting lion (Merlion).
During the post-op period when she felt that pain, she was reading blogs and Instagram posts by other tonsillectomy patients, desperately searching for answers. What she wanted to know was: “Which day does it start getting easier?”
Now, let’s go into detail about the pain Puchiko experienced.
1) Immediate Post-Op Pain
As mentioned, the pain immediately after surgery was minimal. I was truly impressed by the power of general anesthesia. Even though I knew it was thanks to the anesthesia, Puchiko thought, “This is easy!” The pain level was about 1 on a 5-point scale. So, at this point, the pain was nothing for Puchiko to be scared of. To make it clearer, it was about the level of pain when tonsillitis is just starting: “Oh, my throat hurts a bit. I wonder if it’s going to swell up later…”
2) Pain During Eating and Drinking
The pain hits precisely at the moment of swallowing. The first meal starts with soft rice porridge, but it wasn’t tasty. Puchiko already had kidney disease-related dietary restrictions, so she didn’t have much freedom, but if you don’t have such restrictions and can buy food from the convenience store, I recommend jelly and ice cream. Since you know the pain that comes with swallowing, your appetite might decrease, but please eat well and get nutrition to help the scabs form quickly over the tonsil site. And whatever you do, do not eat crackers or cookies, even if they are served, unlike Puchiko!
3) Night Pain and Countermeasures
When Puchiko had her tonsillectomy, she slept with her mouth open without using nasal strips (though she was wearing a mask during this hospital stay…). Other tonsillectomy patients also said that waking up was painful. I recommend you avoid sleeping with mouth breathing to alleviate the pain even slightly. This is also something you should continue doing long-term, as mouth breathing is linked to renal disease. Nasal strips are highly recommended! Puchiko has tried various types, but for times when she absolutely doesn’t want to mouth breathe (like sleeping on a plane or when feeling sick), she uses this specific tape that can be easily torn by hand. Some people also brought humidifying masks containing menthol. I don’t know if they sell them overseas, but a mentholated, humidifying mask helps.
4) Effectiveness of Painkillers
As is common for kidney disease patients, she couldn’t use Loxonin, so Puchiko was prescribed Calonal (acetaminophen). The frequency was strictly controlled; in her case, it was limited to four times a day. This means you can’t just take it whenever you feel pain. Since meals were agonizing, she took it before eating. Calonal can be taken on an empty stomach, so pre-meal was fine. This meant three out of four doses were reserved for before meals. So, when was the last dose? She took it before sleeping. It’s impossible to sleep with the pain. It takes about 15 minutes to kick in, so she timed the intake carefully.
6. Message
To describe the pain: Puchiko said it was basically two or three times the pain of a swollen tonsil. I think “intense” is the right word for it. To her, the pain from the tattoo removal laser and the urinary catheter was worse.
You’re probably thinking, “It hurts, and when will I be free from this pain?” Puchiko felt the same way. For her, the most agonizing pain was the morning after the surgery. She was so irritable that I was almost kicked. By the third day, the pain was perhaps minus 1/20th—it had slightly decreased. But the pain during meals lingered.
If the hospitalization had been for the tonsillectomy alone (not combined with steroid pulse therapy), she would have still been in pain on the day of discharge (which was an 8-day stay for her), and even three days after discharge. She returned to work immediately after being discharged but remembers feeling pain during lunch. However, a week after discharge, it became much, much easier.
Now, she is freed from that miserable pain of having swollen tonsils when she catches a cold. And since people who have tonsils often accumulate pus plugs (tonsil stones), she is now free of them and has clean breath. Think of this pain as borrowing a bit of misery now to pay it back later. The pain gradually, very gradually, decreases day by day. I know you are full of anxiety, but I hope this article will encourage you. We wholeheartedly support you!
You Might Also Like